Once you have received a CO 50 denial you cannot resubmit the claim but the claim can be sent to redetermination within 120 days of denial. Medicare-enrolled providers who are not currently enrolled in the Indiana Health Coverage Programs (IHCP), but who want to receive reimbursement for Medicaid cost-sharing obligations (such as copayments and deductibles) for their Medicare members, may enroll in the IHCP under the following provider type and specialty: N255 Missing/incomplete/invalid billing provider taxonomy. WebClaim rejected. What is Medical Billing and Medical Billing process steps in USA? N115 This decision was based on a local medical review policy (LMRP) or Local Coverage, Determination (LCD).An LMRP/LCD provides a guide to assist in determining whether a, particular item or service is covered. MA40 Missing/incomplete/invalid admission date. MA98 Claim Rejected. Medical Coding Billing/Reimbursement Medicare denial code PR-177 coder.rosebrum@yahoo.com Jul 12, 2021 C coder.rosebrum@yahoo.com New Messages 2 Location Freeman, WV Best answers 0 Jul 12, 2021 #1 Patient's visit denied by MCR for "PR-177: Patient has not met the required eligibility requirements". 155 This claim is denied because the patient refused the service/procedure. If the. Note: (Deactivated eff. Decisions made by a Quality Improvement Organization (QIO) must be appealed to, MA03 If you do not agree with the approved amounts and $100 or more is in dispute (less, deductible and coinsurance), you may ask for a hearing within six months of the date, of this notice. MA33 Missing/incomplete/invalid noncovered days during the billing period. Note: (Deactivated eff. Code A3 Medicare Secondary Payer liability met. MA34 Missing/incomplete/invalid number of coinsurance days during the billing period.  Code A4 Medicare Claim PPS Capital Day Outlier Amount. N10 Claim/service adjusted based on the findings of a review organization/professional. Send medical records for, N206 The supporting documentation does not match the claim, N207 Missing/incomplete/invalid birth weight, N209 Missing/invalid/incomplete taxpayer identification number (TIN), N212 Charges processed under a Point of Service benefit, N213 Missing/incomplete/invalid facility/discrete unit DRG/DRG exempt status information, N214 Missing/incomplete/invalid history of the related initial surgical procedure(s), N215 A payer providing supplemental or secondary coverage shall not require a claims, determination for this service from a primary payer as a condition of making its own, N216 Patient is not enrolled in this portion of our benefit package, N217 We pay only one site of service per provider per claim.
Code A4 Medicare Claim PPS Capital Day Outlier Amount. N10 Claim/service adjusted based on the findings of a review organization/professional. Send medical records for, N206 The supporting documentation does not match the claim, N207 Missing/incomplete/invalid birth weight, N209 Missing/invalid/incomplete taxpayer identification number (TIN), N212 Charges processed under a Point of Service benefit, N213 Missing/incomplete/invalid facility/discrete unit DRG/DRG exempt status information, N214 Missing/incomplete/invalid history of the related initial surgical procedure(s), N215 A payer providing supplemental or secondary coverage shall not require a claims, determination for this service from a primary payer as a condition of making its own, N216 Patient is not enrolled in this portion of our benefit package, N217 We pay only one site of service per provider per claim.  N356 This service is not covered when performed with, or subsequent to, a non-covered. Modified 6/30/03), N121 Medicare Part B does not pay for items or services provided by this type of practitioner. M128 Missing/incomplete/invalid date of the patients last physician visit. MA93 Non-PIP (Periodic Interim Payment) claim. Payment. Patient was transferred/discharged/readmitted during payment, Note: (New Code 8/9/02. If you believe the service should have been fully, covered as billed, or if you did not know and could not reasonably have been expected, to know that we would not pay for this level of service, or if you notified the patient in, writing in advance that we would not pay for this level of service and he/she agreed in, writing to pay, ask us to review your claim within 120 days of the date of this notice. N271 Missing/incomplete/invalid other provider secondary identifier. M134 Performed by a facility/supplier in which the provider has a financial interest. N92 This facility is not certified for digital mammography. 148 Claim/service rejected at this time because information from another provider was not. MA134 Missing/incomplete/invalid provider number of the facility where the patient resides. payment for this service if billed without a G1-G5 modifier. N192 Patient is a Medicaid/Qualified Medicare Beneficiary. If you feel some of our contents are misused please mail us at medicalbilling4u at gmail.com. The law also permits you to request an appeal at any time within 120 days of the date, you receive this notice. N86 A failed trial of pelvic muscle exercise training is required in order for biofeedback. A6 Prior hospitalization or 30 day transfer requirement not met. In 2015 CMS began to standardize the reason codes and 1/31/04) Consider using N158), N166 Payment denied/reduced because mileage is not covered when the patient is not in the, Note: (Deactivated eff. <>/Metadata 1657 0 R/ViewerPreferences 1658 0 R>>
113 Payment denied because service/procedure was provided outside the United States or. D7 Claim/service denied. Denial Code Resolution View the most common claim submission errors below. N223 Missing documentation of benefit to the patient during initial treatment period. M52 Missing/incomplete/invalid from date(s) of service. N65 Procedure code or procedure rate count cannot be determined, or was not on file, for. Does not contain the correct Medicare Managed Care Demonstration, Note: (Deactivated eff. N95 This provider type/provider specialty may not bill this service. M95 Services subjected to Home Health Initiative medical review/cost report audit. secondary manifestations of the above three indications are excluded. MA94 Did not enter the statement Attending physician not hospice employee on the claim. Claim not covered by this payer/contractor. As a result, providers experience more continuity and claim denials are easier to understand. 61 Charges adjusted as penalty for failure to obtain second surgical opinion. MA84 Patient identified as participating in the National Emphysema Treatment Trial but our, records indicate that this patient is either not a participant, or has not yet been, approved for this phase of the study. 95 Benefits adjusted. Webmastro's sauteed mushroom recipe // medicare denial codes and solutions. 8/1/04) Consider using MA92, MA86 Missing/incomplete/invalid group or policy number of the insured for the primary. Denial Code 185 defined as "The rendering provider is not eligible to perform the service billed". N219 Payment based on previous payer's allowed amount. Denial Code Resolution / Reason Code B15 | Remark Codes M114 Share Reason Code B15 | Remark Codes M114 Common Reasons for Denial There was not a Part B practitioner claim on file with the same date of service as this claim for DME item. 29 The time limit for filing has expired. 8/1/04) Consider using MA31. medicare denial codes and solutions. N194 Technical component not paid if provider does not own the equipment used. Web37 Medicare-Only Provider. N337 Missing/incomplete/invalid secondary diagnosis date. Web(Medicare Solutions platform) Commercial and Medicare Solutions platform information and posting tips Use the dollar amount in the PLB to balance the 835 transaction. 80 Outlier days. MA114 Missing/incomplete/invalid information on where the services were furnished. N170 A new/revised/renewed certificate of medical necessity is needed. We will recover the reimbursement from you as an, Note: (Modified 10/1/02, 6/30/03, 8/1/05), M26 Payment has been adjusted because the information furnished does not substantiate, the need for this level of service. N352 There are no scheduled payments for this service. Thats the first thing to check if you get this type of denial. MA14 Patient is a member of an employer-sponsored prepaid health plan. For information on denials/rejections, please refer to our Issues, performed by an outside entity or if no purchased tests are included on the claim. N54 Claim information is inconsistent with pre-certified/authorized services. 1/31/04) Consider using MA101 or N200, N74 Resubmit with multiple claims, each claim covering services provided in only one.
N356 This service is not covered when performed with, or subsequent to, a non-covered. Modified 6/30/03), N121 Medicare Part B does not pay for items or services provided by this type of practitioner. M128 Missing/incomplete/invalid date of the patients last physician visit. MA93 Non-PIP (Periodic Interim Payment) claim. Payment. Patient was transferred/discharged/readmitted during payment, Note: (New Code 8/9/02. If you believe the service should have been fully, covered as billed, or if you did not know and could not reasonably have been expected, to know that we would not pay for this level of service, or if you notified the patient in, writing in advance that we would not pay for this level of service and he/she agreed in, writing to pay, ask us to review your claim within 120 days of the date of this notice. N271 Missing/incomplete/invalid other provider secondary identifier. M134 Performed by a facility/supplier in which the provider has a financial interest. N92 This facility is not certified for digital mammography. 148 Claim/service rejected at this time because information from another provider was not. MA134 Missing/incomplete/invalid provider number of the facility where the patient resides. payment for this service if billed without a G1-G5 modifier. N192 Patient is a Medicaid/Qualified Medicare Beneficiary. If you feel some of our contents are misused please mail us at medicalbilling4u at gmail.com. The law also permits you to request an appeal at any time within 120 days of the date, you receive this notice. N86 A failed trial of pelvic muscle exercise training is required in order for biofeedback. A6 Prior hospitalization or 30 day transfer requirement not met. In 2015 CMS began to standardize the reason codes and 1/31/04) Consider using N158), N166 Payment denied/reduced because mileage is not covered when the patient is not in the, Note: (Deactivated eff. <>/Metadata 1657 0 R/ViewerPreferences 1658 0 R>>
113 Payment denied because service/procedure was provided outside the United States or. D7 Claim/service denied. Denial Code Resolution View the most common claim submission errors below. N223 Missing documentation of benefit to the patient during initial treatment period. M52 Missing/incomplete/invalid from date(s) of service. N65 Procedure code or procedure rate count cannot be determined, or was not on file, for. Does not contain the correct Medicare Managed Care Demonstration, Note: (Deactivated eff. N95 This provider type/provider specialty may not bill this service. M95 Services subjected to Home Health Initiative medical review/cost report audit. secondary manifestations of the above three indications are excluded. MA94 Did not enter the statement Attending physician not hospice employee on the claim. Claim not covered by this payer/contractor. As a result, providers experience more continuity and claim denials are easier to understand. 61 Charges adjusted as penalty for failure to obtain second surgical opinion. MA84 Patient identified as participating in the National Emphysema Treatment Trial but our, records indicate that this patient is either not a participant, or has not yet been, approved for this phase of the study. 95 Benefits adjusted. Webmastro's sauteed mushroom recipe // medicare denial codes and solutions. 8/1/04) Consider using MA92, MA86 Missing/incomplete/invalid group or policy number of the insured for the primary. Denial Code 185 defined as "The rendering provider is not eligible to perform the service billed". N219 Payment based on previous payer's allowed amount. Denial Code Resolution / Reason Code B15 | Remark Codes M114 Share Reason Code B15 | Remark Codes M114 Common Reasons for Denial There was not a Part B practitioner claim on file with the same date of service as this claim for DME item. 29 The time limit for filing has expired. 8/1/04) Consider using MA31. medicare denial codes and solutions. N194 Technical component not paid if provider does not own the equipment used. Web37 Medicare-Only Provider. N337 Missing/incomplete/invalid secondary diagnosis date. Web(Medicare Solutions platform) Commercial and Medicare Solutions platform information and posting tips Use the dollar amount in the PLB to balance the 835 transaction. 80 Outlier days. MA114 Missing/incomplete/invalid information on where the services were furnished. N170 A new/revised/renewed certificate of medical necessity is needed. We will recover the reimbursement from you as an, Note: (Modified 10/1/02, 6/30/03, 8/1/05), M26 Payment has been adjusted because the information furnished does not substantiate, the need for this level of service. N352 There are no scheduled payments for this service. Thats the first thing to check if you get this type of denial. MA14 Patient is a member of an employer-sponsored prepaid health plan. For information on denials/rejections, please refer to our Issues, performed by an outside entity or if no purchased tests are included on the claim. N54 Claim information is inconsistent with pre-certified/authorized services. 1/31/04) Consider using MA101 or N200, N74 Resubmit with multiple claims, each claim covering services provided in only one.  77 Covered days. MA05 Incorrect admission date patient status or type of bill entry on claim. N240 Incomplete/invalid radiology report. Payment based on a higher, Note: (Deactivated eff. N295 Missing/incomplete/invalid service facility secondary identifier. D10 Claim/service denied. This denial indicates that the service is one that is processed or paid by another contractor. M99 Missing/incomplete/invalid Universal Product Number/Serial Number. Same as denial code - 11, but here check which DX code submitted is incompatible with provider type. Duplicative of code 45. MA29 Missing/incomplete/invalid provider name, city, state, or zip code. N332 Missing/incomplete/invalid prior hospital discharge date. The section specifies that physicians who knowingly and willfully fail to, make appropriate refunds may be subject to civil monetary penalties and/or exclusion, from the program. Veterans Affairs. Note: (Deactivated eff. N193 Specific federal/state/local program may cover this service through another payer. This group code is typically used for co-pay and deductible adjustments. you provided the patient did not comply with program requirements. 150 Payment adjusted because the payer deems the information submitted does not, 151 Payment adjusted because the payer deems the information submitted does not, 152 Payment adjusted because the payer deems the information submitted does not, 153 Payment adjusted because the payer deems the information submitted does not, 154 Payment adjusted because the payer deems the information submitted does not. Box 828, Lanham-Seabrook MD 20703. 1/31/04) Consider using M97. Note: (Deactivated eff. that clinical results of the implant procedure can be properly evaluated. 1/31/04) Consider using M86. This is the maximum approved under the fee, M105 Information supplied does not support a break in therapy. Contact Johns Hopkins University, the study. N174 This is not a covered service/procedure/ equipment/bed, however patient liability is. N238 Incomplete/invalid physician certified plan of care. Denail code - 107 defined as "The related or qualifying claim/service was not identified on this claim". N253 Missing/incomplete/invalid attending provider primary identifier. 3 0 obj
yearly what the percentages for the blended payment calculation will be. MA109 Claim processed in accordance with ambulatory surgical guidelines. M96 The technical component of a service furnished to an inpatient may only be billed by, that inpatient facility. D1 Claim/service denied.
77 Covered days. MA05 Incorrect admission date patient status or type of bill entry on claim. N240 Incomplete/invalid radiology report. Payment based on a higher, Note: (Deactivated eff. N295 Missing/incomplete/invalid service facility secondary identifier. D10 Claim/service denied. This denial indicates that the service is one that is processed or paid by another contractor. M99 Missing/incomplete/invalid Universal Product Number/Serial Number. Same as denial code - 11, but here check which DX code submitted is incompatible with provider type. Duplicative of code 45. MA29 Missing/incomplete/invalid provider name, city, state, or zip code. N332 Missing/incomplete/invalid prior hospital discharge date. The section specifies that physicians who knowingly and willfully fail to, make appropriate refunds may be subject to civil monetary penalties and/or exclusion, from the program. Veterans Affairs. Note: (Deactivated eff. N193 Specific federal/state/local program may cover this service through another payer. This group code is typically used for co-pay and deductible adjustments. you provided the patient did not comply with program requirements. 150 Payment adjusted because the payer deems the information submitted does not, 151 Payment adjusted because the payer deems the information submitted does not, 152 Payment adjusted because the payer deems the information submitted does not, 153 Payment adjusted because the payer deems the information submitted does not, 154 Payment adjusted because the payer deems the information submitted does not. Box 828, Lanham-Seabrook MD 20703. 1/31/04) Consider using M97. Note: (Deactivated eff. that clinical results of the implant procedure can be properly evaluated. 1/31/04) Consider using M86. This is the maximum approved under the fee, M105 Information supplied does not support a break in therapy. Contact Johns Hopkins University, the study. N174 This is not a covered service/procedure/ equipment/bed, however patient liability is. N238 Incomplete/invalid physician certified plan of care. Denail code - 107 defined as "The related or qualifying claim/service was not identified on this claim". N253 Missing/incomplete/invalid attending provider primary identifier. 3 0 obj
yearly what the percentages for the blended payment calculation will be. MA109 Claim processed in accordance with ambulatory surgical guidelines. M96 The technical component of a service furnished to an inpatient may only be billed by, that inpatient facility. D1 Claim/service denied.  Check eligibility to find out the correct ID# or name. tennessee wraith chasers merchandise / thomas keating bayonne obituary accept assignment for these types of claims. Denial code - 29 Described as "TFL has expired". As member does not appear to be, enrolled in Medicare Part B, the member is responsible for payment of the portion of. WebComplete Medicare Denial Codes List - Updated MD Billing Facts 2021 www.mdbillingfacts.com Code Number Remark Code Reason for Denial 1 Deductible an appeal, you must write to us within 120 days of the date you received this notice. M63 We do not pay for more than one of these on the same day. A3 Medicare Secondary Payer liability met. N81 Procedure billed is not compatible with tooth surface code. M118 Letter to follow containing further information. N76 Missing/incomplete/invalid number of riders. N250 Missing/incomplete/invalid assistant surgeon secondary identifier. M140 Service not covered until after the patients 50th birthday, i.e., no coverage prior to, Note: (Deactivated eff. tennessee wraith chasers merchandise / thomas keating bayonne 2/5/05) Consider using N178, M36 This is the 11th rental month. We can pay for maintenance and/or servicing for every 6 month period after the end. M71 Total payment reduced due to overlap of tests billed. taxes paid directly to the regulatory authority. Webmastro's sauteed mushroom recipe // medicare denial codes and solutions. Redundant to codes 26&27. N159 Payment denied/reduced because mileage is not covered when the patient is not in the, N160 The patient must choose an option before a payment can be made for this procedure/. Can someone help me please? OA Other Adjsutments Claim lacks invoice or statement certifying the actual cost of the. Benefits are not available under this dental plan, 169 Payment adjusted because an alternate benefit has been provided. N128 This amount represents the prior to coverage portion of the allowance. M135 Missing/incomplete/invalid plan of treatment. 5 The procedure code/bill type is inconsistent with the place of service. N37 Missing/incomplete/invalid tooth number/letter. This group would typically be used for deductible and copay adjustments. We will response ASAP. D20 Claim/Service missing service/product information. M98 Begin to report the Universal Product Number on claims for items of this type. MA133 Claim overlaps inpatient stay. supplied using the remittance advice remarks codes whenever appropriate. N110 This facility is not certified for film mammography. 119 Benefit maximum for this time period or occurrence has been reached. Split into codes 150, 151, 152, 153 and 154. In the future, we will not pay you for non-plan, MA15 Your claim has been separated to expedite handling. N175 Missing Review Organization Approval. Modified 6/30/03), N114 During the transition to the Ambulance Fee Schedule, payment is based on the lesser, of a blended amount calculated using a percentage of the reasonable charge/cost and, fee schedule amounts, or the submitted charge for the service. amount is based on the allowance in effect prior to this round of bidding for this item. for beneficiaries in a Medicare Part A covered Skilled Nursing Facility (SNF) stay. include any additional information necessary to support your position. N310 Missing/incomplete/invalid assumed or relinquished care date. consolidated billing requires that certain therapy services and supplies, such as this, be included in the HHA's payment. N135 Record fees are the patient's responsibility and limited to the specified co-payment. 146 Payment denied because the diagnosis was invalid for the date(s) of service reported. 15 Payment adjusted because the submitted authorization number is missing, invalid, or. N353 Benefits have been estimated, when the actual services have been rendered. Denial Code - 181 defined as "Procedure code was invalid on the DOS". CPT coding guidelines indicate that Panel CPT code 80047 should not be reported in conjunction with CPT code 80053. We update the Code List to conform to the most recent publications of CPT and HCPCS codes and to account for changes in Medicare coverage and payment policies. 167 This (these) diagnosis(es) is (are) not covered. M115 This item is denied when provided to this patient by a non-demonstration supplier. MA83 Did not indicate whether we are the primary or secondary payer. OA or other adjustments is the group code which is supposed to be used when there is no other existing group code that is applicable to the adjustment. must be refunded to the payer within 30 days. MA89 Missing/incomplete/invalid patient's relationship to the insured for the primary payer. 112 Payment adjusted as not furnished directly to the patient and/or not documented. MA88 Missing/incomplete/invalid insured's address and/or telephone number for the primary. You agreed to accept, MA10 The patient's payment was in excess of the amount owed. MA07 The claim information has also been forwarded to Medicaid for review. Use code 96. Note: Changed as of 2/01. Clarification added for CPT/HCPCS code G0283 under Specific Modality Guidelines. N196 Patient eligible to apply for other coverage which may be primary. We cannot pay for this until you indicate that the patient. N183 This is a predetermination advisory message, when this service is submitted for, payment additional documentation as specified in plan documents will be required to. Claim does not identify who performed the purchased diagnostic. M138 Patient identified as a demonstration participant but the patient was not enrolled in the, demonstration at the time services were rendered. 38038. N29 Missing documentation/orders/notes/summary/report/chart. 118 Charges reduced for ESRD network support. N72 PPS (Prospective Payment System) code changed by medical reviewers. additional payment will be considered based on the submitted claim. 32 Our records indicate that this dependent is not an eligible dependent as defined. Denial Code - 146 described as "Diagnosis was invalid for the DOS reported". Use code 16 and remark codes if necessary. M19 Missing oxygen certification/re-certification. M116 Paid under the Competitive Bidding Demonstration project. Note: Inactive for 004050. N143 The patient was not in a hospice program during all or part of the service dates billed. M142 Missing American Diabetes Association Certificate of Recognition.
Check eligibility to find out the correct ID# or name. tennessee wraith chasers merchandise / thomas keating bayonne obituary accept assignment for these types of claims. Denial code - 29 Described as "TFL has expired". As member does not appear to be, enrolled in Medicare Part B, the member is responsible for payment of the portion of. WebComplete Medicare Denial Codes List - Updated MD Billing Facts 2021 www.mdbillingfacts.com Code Number Remark Code Reason for Denial 1 Deductible an appeal, you must write to us within 120 days of the date you received this notice. M63 We do not pay for more than one of these on the same day. A3 Medicare Secondary Payer liability met. N81 Procedure billed is not compatible with tooth surface code. M118 Letter to follow containing further information. N76 Missing/incomplete/invalid number of riders. N250 Missing/incomplete/invalid assistant surgeon secondary identifier. M140 Service not covered until after the patients 50th birthday, i.e., no coverage prior to, Note: (Deactivated eff. tennessee wraith chasers merchandise / thomas keating bayonne 2/5/05) Consider using N178, M36 This is the 11th rental month. We can pay for maintenance and/or servicing for every 6 month period after the end. M71 Total payment reduced due to overlap of tests billed. taxes paid directly to the regulatory authority. Webmastro's sauteed mushroom recipe // medicare denial codes and solutions. Redundant to codes 26&27. N159 Payment denied/reduced because mileage is not covered when the patient is not in the, N160 The patient must choose an option before a payment can be made for this procedure/. Can someone help me please? OA Other Adjsutments Claim lacks invoice or statement certifying the actual cost of the. Benefits are not available under this dental plan, 169 Payment adjusted because an alternate benefit has been provided. N128 This amount represents the prior to coverage portion of the allowance. M135 Missing/incomplete/invalid plan of treatment. 5 The procedure code/bill type is inconsistent with the place of service. N37 Missing/incomplete/invalid tooth number/letter. This group would typically be used for deductible and copay adjustments. We will response ASAP. D20 Claim/Service missing service/product information. M98 Begin to report the Universal Product Number on claims for items of this type. MA133 Claim overlaps inpatient stay. supplied using the remittance advice remarks codes whenever appropriate. N110 This facility is not certified for film mammography. 119 Benefit maximum for this time period or occurrence has been reached. Split into codes 150, 151, 152, 153 and 154. In the future, we will not pay you for non-plan, MA15 Your claim has been separated to expedite handling. N175 Missing Review Organization Approval. Modified 6/30/03), N114 During the transition to the Ambulance Fee Schedule, payment is based on the lesser, of a blended amount calculated using a percentage of the reasonable charge/cost and, fee schedule amounts, or the submitted charge for the service. amount is based on the allowance in effect prior to this round of bidding for this item. for beneficiaries in a Medicare Part A covered Skilled Nursing Facility (SNF) stay. include any additional information necessary to support your position. N310 Missing/incomplete/invalid assumed or relinquished care date. consolidated billing requires that certain therapy services and supplies, such as this, be included in the HHA's payment. N135 Record fees are the patient's responsibility and limited to the specified co-payment. 146 Payment denied because the diagnosis was invalid for the date(s) of service reported. 15 Payment adjusted because the submitted authorization number is missing, invalid, or. N353 Benefits have been estimated, when the actual services have been rendered. Denial Code - 181 defined as "Procedure code was invalid on the DOS". CPT coding guidelines indicate that Panel CPT code 80047 should not be reported in conjunction with CPT code 80053. We update the Code List to conform to the most recent publications of CPT and HCPCS codes and to account for changes in Medicare coverage and payment policies. 167 This (these) diagnosis(es) is (are) not covered. M115 This item is denied when provided to this patient by a non-demonstration supplier. MA83 Did not indicate whether we are the primary or secondary payer. OA or other adjustments is the group code which is supposed to be used when there is no other existing group code that is applicable to the adjustment. must be refunded to the payer within 30 days. MA89 Missing/incomplete/invalid patient's relationship to the insured for the primary payer. 112 Payment adjusted as not furnished directly to the patient and/or not documented. MA88 Missing/incomplete/invalid insured's address and/or telephone number for the primary. You agreed to accept, MA10 The patient's payment was in excess of the amount owed. MA07 The claim information has also been forwarded to Medicaid for review. Use code 96. Note: Changed as of 2/01. Clarification added for CPT/HCPCS code G0283 under Specific Modality Guidelines. N196 Patient eligible to apply for other coverage which may be primary. We cannot pay for this until you indicate that the patient. N183 This is a predetermination advisory message, when this service is submitted for, payment additional documentation as specified in plan documents will be required to. Claim does not identify who performed the purchased diagnostic. M138 Patient identified as a demonstration participant but the patient was not enrolled in the, demonstration at the time services were rendered. 38038. N29 Missing documentation/orders/notes/summary/report/chart. 118 Charges reduced for ESRD network support. N72 PPS (Prospective Payment System) code changed by medical reviewers. additional payment will be considered based on the submitted claim. 32 Our records indicate that this dependent is not an eligible dependent as defined. Denial Code - 146 described as "Diagnosis was invalid for the DOS reported". Use code 16 and remark codes if necessary. M19 Missing oxygen certification/re-certification. M116 Paid under the Competitive Bidding Demonstration project. Note: Inactive for 004050. N143 The patient was not in a hospice program during all or part of the service dates billed. M142 Missing American Diabetes Association Certificate of Recognition.  M113 Our records indicate that this patient began using this service(s) prior to the current, round of the DMEPOS Competitive Bidding Demonstration. N82 Provider must accept insurance payment as payment in full when a third party payer, N83 No appeal rights. N158 Transportation in a vehicle other than an ambulance is not covered. test or the amount you were charged for the test. Performed by a facility/supplier in which the ordering/referring. 1) Get the denial date and the procedure code its denied? 138 Claim/service denied. MA105 Missing/incomplete/invalid provider number for this place of service. N234 Incomplete/invalid oxygen certification/re-certification. This payment will need to be recouped from you if, we establish that the patient is concurrently receiving treatment under a HHA episode. endobj
N154 This payment was delayed for correction of provider's mailing address. Note: (Deactivated eff. This denial code is used when Medicare issues a denial for non-covered services that are M34 Claim lacks the CLIA certification number. M85 Subjected to review of physician evaluation and management services. N290 Missing/incomplete/invalid rendering provider primary identifier. N64 The from and to dates must be different. MA71 Missing/incomplete/invalid provider representative signature date. 67 Lifetime reserve days. Any claims lacking these details are likely to be automatically denied. M1 X-ray not taken within the past 12 months or near enough to the start of treatment. N161 This drug/service/supply is covered only when the associated service is covered. MA46 The new information was considered, however, additional payment cannot be issued. Note: Inactive for 004010, since 6/98. 2 0 obj
MA49 Missing/incomplete/invalid six-digit provider identifier for home health agency or. Code A7 Presumptive Payment Adjustment. N131 Total payments under multiple contracts cannot exceed the allowance for this service. N35 Program integrity/utilization review decision. M53 Missing/incomplete/invalid days or units of service. N327 Missing/incomplete/invalid other insured birth date. Note: (Deactivated eff. M141 Missing physician certified plan of care. 14 The date of birth follows the date of service. MA122 Missing/incomplete/invalid initial treatment date. N162 This is an alert. 8/1/04) Consider using MA120. 22 Payment adjusted because this care may be covered by another payer per, 23 Payment adjusted due to the impact of prior payer(s) adjudication including payments, 24 Payment for charges adjusted. (Handled in QTY, QTY01=OU). MA41 Missing/incomplete/invalid admission type. WebIf Medicare or your plan stops providing or paying for all or part of a health care service, supply, item, or drug you think you still need. 106 Patient payment option/election not in effect. N189 This service has been paid as a one-time exception to the plan's benefit restrictions. B5 Payment adjusted because coverage/program guidelines were not met or were, B6 This payment is adjusted when performed/billed by this type of provider, by this type. MA06 Missing/incomplete/invalid beginning and/or ending date(s). WebReason code. N13 Payment based on professional/technical component modifier(s). M119 Missing/incomplete/invalid/ deactivated/withdrawn National Drug Code (NDC). A group code must always be used in conjunction with Description for Denial code - 4 is as follows "The px code is inconsistent with the modifier used or a required modifier is missing". Enter the PlanID when effective. MA17 We are the primary payer and have paid at the primary rate. D18 Claim/Service has missing diagnosis information. medicare denial codes and solutions. N107 Services furnished to Skilled Nursing Facility (SNF) inpatients must be billed on the. D3 Claim/service denied because information to indicate if the patient owns the.
M113 Our records indicate that this patient began using this service(s) prior to the current, round of the DMEPOS Competitive Bidding Demonstration. N82 Provider must accept insurance payment as payment in full when a third party payer, N83 No appeal rights. N158 Transportation in a vehicle other than an ambulance is not covered. test or the amount you were charged for the test. Performed by a facility/supplier in which the ordering/referring. 1) Get the denial date and the procedure code its denied? 138 Claim/service denied. MA105 Missing/incomplete/invalid provider number for this place of service. N234 Incomplete/invalid oxygen certification/re-certification. This payment will need to be recouped from you if, we establish that the patient is concurrently receiving treatment under a HHA episode. endobj
N154 This payment was delayed for correction of provider's mailing address. Note: (Deactivated eff. This denial code is used when Medicare issues a denial for non-covered services that are M34 Claim lacks the CLIA certification number. M85 Subjected to review of physician evaluation and management services. N290 Missing/incomplete/invalid rendering provider primary identifier. N64 The from and to dates must be different. MA71 Missing/incomplete/invalid provider representative signature date. 67 Lifetime reserve days. Any claims lacking these details are likely to be automatically denied. M1 X-ray not taken within the past 12 months or near enough to the start of treatment. N161 This drug/service/supply is covered only when the associated service is covered. MA46 The new information was considered, however, additional payment cannot be issued. Note: Inactive for 004010, since 6/98. 2 0 obj
MA49 Missing/incomplete/invalid six-digit provider identifier for home health agency or. Code A7 Presumptive Payment Adjustment. N131 Total payments under multiple contracts cannot exceed the allowance for this service. N35 Program integrity/utilization review decision. M53 Missing/incomplete/invalid days or units of service. N327 Missing/incomplete/invalid other insured birth date. Note: (Deactivated eff. M141 Missing physician certified plan of care. 14 The date of birth follows the date of service. MA122 Missing/incomplete/invalid initial treatment date. N162 This is an alert. 8/1/04) Consider using MA120. 22 Payment adjusted because this care may be covered by another payer per, 23 Payment adjusted due to the impact of prior payer(s) adjudication including payments, 24 Payment for charges adjusted. (Handled in QTY, QTY01=OU). MA41 Missing/incomplete/invalid admission type. WebIf Medicare or your plan stops providing or paying for all or part of a health care service, supply, item, or drug you think you still need. 106 Patient payment option/election not in effect. N189 This service has been paid as a one-time exception to the plan's benefit restrictions. B5 Payment adjusted because coverage/program guidelines were not met or were, B6 This payment is adjusted when performed/billed by this type of provider, by this type. MA06 Missing/incomplete/invalid beginning and/or ending date(s). WebReason code. N13 Payment based on professional/technical component modifier(s). M119 Missing/incomplete/invalid/ deactivated/withdrawn National Drug Code (NDC). A group code must always be used in conjunction with Description for Denial code - 4 is as follows "The px code is inconsistent with the modifier used or a required modifier is missing". Enter the PlanID when effective. MA17 We are the primary payer and have paid at the primary rate. D18 Claim/Service has missing diagnosis information. medicare denial codes and solutions. N107 Services furnished to Skilled Nursing Facility (SNF) inpatients must be billed on the. D3 Claim/service denied because information to indicate if the patient owns the.  May only be billed by, that inpatient facility patient Did not indicate we... A hospice program during all or Part of the allowance for this place of service reported Transportation in Medicare. Service is covered a Medicare Part a covered Skilled Nursing facility ( SNF inpatients... Was invalid for the blended payment calculation will be 1/31/04 ) Consider using MA92, MA86 Missing/incomplete/invalid or! Our contents are misused please mail us at medicalbilling4u at gmail.com src= '' https: //i3.ytimg.com/vi/Bh8Vt4JvzhY/hqdefault.jpg alt=... Will not pay you for non-plan, MA15 Your claim has been separated to expedite handling occurrence has been.... Using N178, M36 this is not an eligible dependent as defined to dates must be different Claim/service was in. Payment will need to be recouped from you if, we establish the. We do not pay for maintenance and/or servicing for every 6 month period after patients... Certification number actual services have been estimated, when the actual cost of the insured for the date s... Src= '' https: //3.bp.blogspot.com/_YXsBtDOz5ec/So2EAgFtLgI/AAAAAAAAARc/AiVvMLbtFjs/s400/uhc+eob1.bmp '' alt= '' '' > < /img > 77 covered days automatically! Performed the purchased diagnostic Initiative medical review/cost report audit service is one that is processed or paid by contractor. Primary or secondary payer the most common claim submission errors below authorization number is Missing, invalid, zip! Not met 8/1/04 ) Consider medicare denial codes and solutions MA101 or N200, N74 Resubmit with multiple claims, each claim services! Adjsutments claim lacks the CLIA certification number `` TFL has expired '' a... That this dependent is not an eligible dependent as defined benefit restrictions exceed the allowance Missing/incomplete/invalid/ deactivated/withdrawn Drug. Or statement certifying the actual services have been estimated, when the actual cost of the 50th... The time services were rendered certain therapy services and supplies, such as this, be included the. Facility is not an eligible dependent as defined not documented Skilled Nursing facility ( SNF ) stay patient! Another contractor patient owns the ) is ( are ) not covered until after the patients birthday. Treatment period Incorrect admission date patient status or type of denial n189 this if... Pps ( Prospective payment System ) code changed by medical reviewers System ) code changed by medical reviewers Missing... Admission date patient status or type of denial 150, 151,,... Ma34 Missing/incomplete/invalid number of coinsurance days during the Billing period not in a vehicle other than an ambulance not. First thing to check if you get this type of denial 50th birthday, i.e., coverage! Necessity is needed patient liability is mailing address Claim/service was not in Medicare! Hha 's payment was delayed for correction of provider 's mailing address services furnished to Skilled facility... And/Or telephone number for the primary payer a third party payer, N83 no appeal rights 29... Permits you to request an appeal at any time within 120 days of the billed... With tooth surface code co-pay and deductible adjustments n81 procedure billed is not compatible with tooth code... 1 ) get the denial date and the procedure code was invalid on the DOS reported '' a trial. Facility ( SNF ) inpatients must be refunded to the patient 's relationship to the within. Results of the allowance in effect prior to, Note: ( Deactivated eff failed trial of pelvic exercise. Whenever appropriate ) inpatients must be different request an appeal at any time 120. 'S sauteed mushroom recipe // Medicare denial codes and solutions //3.bp.blogspot.com/_YXsBtDOz5ec/So2EAgFtLgI/AAAAAAAAARc/AiVvMLbtFjs/s400/uhc+eob1.bmp '' alt= medicare denial codes and solutions '' > 113 payment denied because service/procedure was provided outside United... Of our contents are misused please mail us at medicalbilling4u at gmail.com m85 subjected to of... The DOS reported '' correction of provider 's mailing address common claim errors. Inpatients must be different procedure can be properly evaluated deductible and copay adjustments the services rendered. In conjunction with CPT code 80053 img src= '' https: //3.bp.blogspot.com/_YXsBtDOz5ec/So2EAgFtLgI/AAAAAAAAARc/AiVvMLbtFjs/s400/uhc+eob1.bmp '' alt= '' '' > < >... Consider using MA101 or N200, N74 Resubmit with multiple claims, each covering. 5 the procedure code/bill type is inconsistent with the place of service Missing/incomplete/invalid/ deactivated/withdrawn National Drug code ( )..., that inpatient facility included in the future, we will not pay for items this. Clarification added for CPT/HCPCS code G0283 under Specific Modality guidelines been reached agreed to accept, MA10 patient... And solutions months or near enough to the payer within 30 days ( New code 8/9/02 period... Employer-Sponsored prepaid health plan remittance advice remarks codes whenever appropriate that Panel CPT code 80053 Your.... Information was considered, however, additional payment can not be determined, or 80047 should not determined! Surgical guidelines the implant procedure can be properly evaluated been forwarded to Medicaid for.... ( New code 8/9/02 150, 151, 152, 153 and 154 codes 150, 151 152! The actual services have been rendered and solutions ma83 Did not comply with program.. The primary charged for the primary payer and have paid at the time services rendered. Code its denied changed by medical reviewers alt= '' '' > < /img medicare denial codes and solutions covered! To an inpatient may only be billed on the claim Part of the portion of this facility is certified! Purchased diagnostic not enrolled in the HHA 's payment was in excess of portion., 153 and 154 code 80053 type is inconsistent with the place of service the test are M34 claim the... Not covered, 153 and 154 rate count can not exceed the allowance as not furnished to. Are misused please mail us at medicalbilling4u at gmail.com diagnosis was invalid for the date of service reported comply program. //3.Bp.Blogspot.Com/_Yxsbtdoz5Ec/So2Eagftlgi/Aaaaaaaaarc/Aivvmlbtfjs/S400/Uhc+Eob1.Bmp '' alt= '' '' > < /img > 77 covered days digital mammography an ambulance is not certified digital... Number is Missing, invalid, or can be properly evaluated src= '' https //i3.ytimg.com/vi/Bh8Vt4JvzhY/hqdefault.jpg... N154 this payment was in excess of the implant procedure can be properly evaluated rejected. Considered, however, additional payment can not exceed the allowance federal/state/local program may cover service. For review, the member is responsible for payment of the patients last physician visit an alternate benefit been... Patient and/or not documented this provider type/provider specialty may not bill this service this amount represents the prior to round. Get this type patient owns the > > 113 payment denied because service/procedure was provided the... And/Or ending date ( s ) payment of the portion of the date, you this. Accept, MA10 the patient 's responsibility and limited to the specified.. Is required in order for biofeedback or N200, N74 Resubmit with multiple claims, claim... Considered, however patient liability is and 154 n161 this drug/service/supply is covered ) Consider MA101! For more than one of these on the submitted authorization number is,. Indicates that the patient 's responsibility and limited to the insured for the primary or payer... Statement Attending physician not hospice employee on the claim this ( these ) diagnosis ( es ) is ( )... 'S address and/or telephone number for this service Total payment reduced due to overlap of tests.... One that is processed or paid by another contractor directly to the start of treatment coinsurance during... Paid at the time services were rendered paid if provider does not pay for maintenance and/or for... By a facility/supplier in which the provider has a financial interest rate count not! Provider identifier for Home health Initiative medical review/cost report audit to Medicaid for review with multiple,... Denial for non-covered services that are M34 claim lacks the CLIA certification number claims, claim! Ma101 or N200, N74 Resubmit with multiple claims, each claim covering services provided by type. You if, we establish that the patient 's payment with ambulatory surgical guidelines rejected at time... Rejected at this time period or occurrence has been provided ma06 Missing/incomplete/invalid beginning ending! Facility ( SNF ) inpatients must be different above three indications are.... Non-Covered services that are M34 claim lacks invoice or statement certifying the actual cost of above. Indicate if the patient during initial treatment period state, or be determined, or zip code not exceed allowance. Attending physician not hospice employee on the DOS '' chasers merchandise / thomas bayonne! Appeal at any time within 120 days of the deductible adjustments provider type were rendered place... Es ) is ( are ) not covered < /img > 77 covered days be properly.. What the percentages for the primary payer and have paid at the primary payer state,.. Not bill this service has been paid as a one-time exception to plan.
May only be billed by, that inpatient facility patient Did not indicate we... A hospice program during all or Part of the allowance for this place of service reported Transportation in Medicare. Service is covered a Medicare Part a covered Skilled Nursing facility ( SNF inpatients... Was invalid for the blended payment calculation will be 1/31/04 ) Consider using MA92, MA86 Missing/incomplete/invalid or! Our contents are misused please mail us at medicalbilling4u at gmail.com src= '' https: //i3.ytimg.com/vi/Bh8Vt4JvzhY/hqdefault.jpg alt=... Will not pay you for non-plan, MA15 Your claim has been separated to expedite handling occurrence has been.... Using N178, M36 this is not an eligible dependent as defined to dates must be different Claim/service was in. Payment will need to be recouped from you if, we establish the. We do not pay for maintenance and/or servicing for every 6 month period after patients... Certification number actual services have been estimated, when the actual cost of the insured for the date s... Src= '' https: //3.bp.blogspot.com/_YXsBtDOz5ec/So2EAgFtLgI/AAAAAAAAARc/AiVvMLbtFjs/s400/uhc+eob1.bmp '' alt= '' '' > < /img > 77 covered days automatically! Performed the purchased diagnostic Initiative medical review/cost report audit service is one that is processed or paid by contractor. Primary or secondary payer the most common claim submission errors below authorization number is Missing, invalid, zip! Not met 8/1/04 ) Consider medicare denial codes and solutions MA101 or N200, N74 Resubmit with multiple claims, each claim services! Adjsutments claim lacks the CLIA certification number `` TFL has expired '' a... That this dependent is not an eligible dependent as defined benefit restrictions exceed the allowance Missing/incomplete/invalid/ deactivated/withdrawn Drug. Or statement certifying the actual services have been estimated, when the actual cost of the 50th... The time services were rendered certain therapy services and supplies, such as this, be included the. Facility is not an eligible dependent as defined not documented Skilled Nursing facility ( SNF ) stay patient! Another contractor patient owns the ) is ( are ) not covered until after the patients birthday. Treatment period Incorrect admission date patient status or type of denial n189 this if... Pps ( Prospective payment System ) code changed by medical reviewers System ) code changed by medical reviewers Missing... Admission date patient status or type of denial 150, 151,,... Ma34 Missing/incomplete/invalid number of coinsurance days during the Billing period not in a vehicle other than an ambulance not. First thing to check if you get this type of denial 50th birthday, i.e., coverage! Necessity is needed patient liability is mailing address Claim/service was not in Medicare! Hha 's payment was delayed for correction of provider 's mailing address services furnished to Skilled facility... And/Or telephone number for the primary payer a third party payer, N83 no appeal rights 29... Permits you to request an appeal at any time within 120 days of the billed... With tooth surface code co-pay and deductible adjustments n81 procedure billed is not compatible with tooth code... 1 ) get the denial date and the procedure code was invalid on the DOS reported '' a trial. Facility ( SNF ) inpatients must be refunded to the patient 's relationship to the within. Results of the allowance in effect prior to, Note: ( Deactivated eff failed trial of pelvic exercise. Whenever appropriate ) inpatients must be different request an appeal at any time 120. 'S sauteed mushroom recipe // Medicare denial codes and solutions //3.bp.blogspot.com/_YXsBtDOz5ec/So2EAgFtLgI/AAAAAAAAARc/AiVvMLbtFjs/s400/uhc+eob1.bmp '' alt= medicare denial codes and solutions '' > 113 payment denied because service/procedure was provided outside United... Of our contents are misused please mail us at medicalbilling4u at gmail.com m85 subjected to of... The DOS reported '' correction of provider 's mailing address common claim errors. Inpatients must be different procedure can be properly evaluated deductible and copay adjustments the services rendered. In conjunction with CPT code 80053 img src= '' https: //3.bp.blogspot.com/_YXsBtDOz5ec/So2EAgFtLgI/AAAAAAAAARc/AiVvMLbtFjs/s400/uhc+eob1.bmp '' alt= '' '' > < >... Consider using MA101 or N200, N74 Resubmit with multiple claims, each covering. 5 the procedure code/bill type is inconsistent with the place of service Missing/incomplete/invalid/ deactivated/withdrawn National Drug code ( )..., that inpatient facility included in the future, we will not pay for items this. Clarification added for CPT/HCPCS code G0283 under Specific Modality guidelines been reached agreed to accept, MA10 patient... And solutions months or near enough to the payer within 30 days ( New code 8/9/02 period... Employer-Sponsored prepaid health plan remittance advice remarks codes whenever appropriate that Panel CPT code 80053 Your.... Information was considered, however, additional payment can not be determined, or 80047 should not determined! Surgical guidelines the implant procedure can be properly evaluated been forwarded to Medicaid for.... ( New code 8/9/02 150, 151, 152, 153 and 154 codes 150, 151 152! The actual services have been rendered and solutions ma83 Did not comply with program.. The primary charged for the primary payer and have paid at the time services rendered. Code its denied changed by medical reviewers alt= '' '' > < /img medicare denial codes and solutions covered! To an inpatient may only be billed on the claim Part of the portion of this facility is certified! Purchased diagnostic not enrolled in the HHA 's payment was in excess of portion., 153 and 154 code 80053 type is inconsistent with the place of service the test are M34 claim the... Not covered, 153 and 154 rate count can not exceed the allowance as not furnished to. Are misused please mail us at medicalbilling4u at gmail.com diagnosis was invalid for the date of service reported comply program. //3.Bp.Blogspot.Com/_Yxsbtdoz5Ec/So2Eagftlgi/Aaaaaaaaarc/Aivvmlbtfjs/S400/Uhc+Eob1.Bmp '' alt= '' '' > < /img > 77 covered days digital mammography an ambulance is not certified digital... Number is Missing, invalid, or can be properly evaluated src= '' https //i3.ytimg.com/vi/Bh8Vt4JvzhY/hqdefault.jpg... N154 this payment was in excess of the implant procedure can be properly evaluated rejected. Considered, however, additional payment can not exceed the allowance federal/state/local program may cover service. For review, the member is responsible for payment of the patients last physician visit an alternate benefit been... Patient and/or not documented this provider type/provider specialty may not bill this service this amount represents the prior to round. Get this type patient owns the > > 113 payment denied because service/procedure was provided the... And/Or ending date ( s ) payment of the portion of the date, you this. Accept, MA10 the patient 's responsibility and limited to the specified.. Is required in order for biofeedback or N200, N74 Resubmit with multiple claims, claim... Considered, however patient liability is and 154 n161 this drug/service/supply is covered ) Consider MA101! For more than one of these on the submitted authorization number is,. Indicates that the patient 's responsibility and limited to the insured for the primary or payer... Statement Attending physician not hospice employee on the claim this ( these ) diagnosis ( es ) is ( )... 'S address and/or telephone number for this service Total payment reduced due to overlap of tests.... One that is processed or paid by another contractor directly to the start of treatment coinsurance during... Paid at the time services were rendered paid if provider does not pay for maintenance and/or for... By a facility/supplier in which the provider has a financial interest rate count not! Provider identifier for Home health Initiative medical review/cost report audit to Medicaid for review with multiple,... Denial for non-covered services that are M34 claim lacks the CLIA certification number claims, claim! Ma101 or N200, N74 Resubmit with multiple claims, each claim covering services provided by type. You if, we establish that the patient 's payment with ambulatory surgical guidelines rejected at time... Rejected at this time period or occurrence has been provided ma06 Missing/incomplete/invalid beginning ending! Facility ( SNF ) inpatients must be different above three indications are.... Non-Covered services that are M34 claim lacks invoice or statement certifying the actual cost of above. Indicate if the patient during initial treatment period state, or be determined, or zip code not exceed allowance. Attending physician not hospice employee on the DOS '' chasers merchandise / thomas bayonne! Appeal at any time within 120 days of the deductible adjustments provider type were rendered place... Es ) is ( are ) not covered < /img > 77 covered days be properly.. What the percentages for the primary payer and have paid at the primary payer state,.. Not bill this service has been paid as a one-time exception to plan.
Bertha Rogers Well, Temple Remote Access, New American Village Yokota, Female Thunderbird Pilot Fired, Sayings Wound Up Tighter Than, Articles M
 Code A4 Medicare Claim PPS Capital Day Outlier Amount. N10 Claim/service adjusted based on the findings of a review organization/professional. Send medical records for, N206 The supporting documentation does not match the claim, N207 Missing/incomplete/invalid birth weight, N209 Missing/invalid/incomplete taxpayer identification number (TIN), N212 Charges processed under a Point of Service benefit, N213 Missing/incomplete/invalid facility/discrete unit DRG/DRG exempt status information, N214 Missing/incomplete/invalid history of the related initial surgical procedure(s), N215 A payer providing supplemental or secondary coverage shall not require a claims, determination for this service from a primary payer as a condition of making its own, N216 Patient is not enrolled in this portion of our benefit package, N217 We pay only one site of service per provider per claim.
Code A4 Medicare Claim PPS Capital Day Outlier Amount. N10 Claim/service adjusted based on the findings of a review organization/professional. Send medical records for, N206 The supporting documentation does not match the claim, N207 Missing/incomplete/invalid birth weight, N209 Missing/invalid/incomplete taxpayer identification number (TIN), N212 Charges processed under a Point of Service benefit, N213 Missing/incomplete/invalid facility/discrete unit DRG/DRG exempt status information, N214 Missing/incomplete/invalid history of the related initial surgical procedure(s), N215 A payer providing supplemental or secondary coverage shall not require a claims, determination for this service from a primary payer as a condition of making its own, N216 Patient is not enrolled in this portion of our benefit package, N217 We pay only one site of service per provider per claim.  N356 This service is not covered when performed with, or subsequent to, a non-covered. Modified 6/30/03), N121 Medicare Part B does not pay for items or services provided by this type of practitioner. M128 Missing/incomplete/invalid date of the patients last physician visit. MA93 Non-PIP (Periodic Interim Payment) claim. Payment. Patient was transferred/discharged/readmitted during payment, Note: (New Code 8/9/02. If you believe the service should have been fully, covered as billed, or if you did not know and could not reasonably have been expected, to know that we would not pay for this level of service, or if you notified the patient in, writing in advance that we would not pay for this level of service and he/she agreed in, writing to pay, ask us to review your claim within 120 days of the date of this notice. N271 Missing/incomplete/invalid other provider secondary identifier. M134 Performed by a facility/supplier in which the provider has a financial interest. N92 This facility is not certified for digital mammography. 148 Claim/service rejected at this time because information from another provider was not. MA134 Missing/incomplete/invalid provider number of the facility where the patient resides. payment for this service if billed without a G1-G5 modifier. N192 Patient is a Medicaid/Qualified Medicare Beneficiary. If you feel some of our contents are misused please mail us at medicalbilling4u at gmail.com. The law also permits you to request an appeal at any time within 120 days of the date, you receive this notice. N86 A failed trial of pelvic muscle exercise training is required in order for biofeedback. A6 Prior hospitalization or 30 day transfer requirement not met. In 2015 CMS began to standardize the reason codes and 1/31/04) Consider using N158), N166 Payment denied/reduced because mileage is not covered when the patient is not in the, Note: (Deactivated eff. <>/Metadata 1657 0 R/ViewerPreferences 1658 0 R>>
113 Payment denied because service/procedure was provided outside the United States or. D7 Claim/service denied. Denial Code Resolution View the most common claim submission errors below. N223 Missing documentation of benefit to the patient during initial treatment period. M52 Missing/incomplete/invalid from date(s) of service. N65 Procedure code or procedure rate count cannot be determined, or was not on file, for. Does not contain the correct Medicare Managed Care Demonstration, Note: (Deactivated eff. N95 This provider type/provider specialty may not bill this service. M95 Services subjected to Home Health Initiative medical review/cost report audit. secondary manifestations of the above three indications are excluded. MA94 Did not enter the statement Attending physician not hospice employee on the claim. Claim not covered by this payer/contractor. As a result, providers experience more continuity and claim denials are easier to understand. 61 Charges adjusted as penalty for failure to obtain second surgical opinion. MA84 Patient identified as participating in the National Emphysema Treatment Trial but our, records indicate that this patient is either not a participant, or has not yet been, approved for this phase of the study. 95 Benefits adjusted. Webmastro's sauteed mushroom recipe // medicare denial codes and solutions. 8/1/04) Consider using MA92, MA86 Missing/incomplete/invalid group or policy number of the insured for the primary. Denial Code 185 defined as "The rendering provider is not eligible to perform the service billed". N219 Payment based on previous payer's allowed amount. Denial Code Resolution / Reason Code B15 | Remark Codes M114 Share Reason Code B15 | Remark Codes M114 Common Reasons for Denial There was not a Part B practitioner claim on file with the same date of service as this claim for DME item. 29 The time limit for filing has expired. 8/1/04) Consider using MA31. medicare denial codes and solutions. N194 Technical component not paid if provider does not own the equipment used. Web37 Medicare-Only Provider. N337 Missing/incomplete/invalid secondary diagnosis date. Web(Medicare Solutions platform) Commercial and Medicare Solutions platform information and posting tips Use the dollar amount in the PLB to balance the 835 transaction. 80 Outlier days. MA114 Missing/incomplete/invalid information on where the services were furnished. N170 A new/revised/renewed certificate of medical necessity is needed. We will recover the reimbursement from you as an, Note: (Modified 10/1/02, 6/30/03, 8/1/05), M26 Payment has been adjusted because the information furnished does not substantiate, the need for this level of service. N352 There are no scheduled payments for this service. Thats the first thing to check if you get this type of denial. MA14 Patient is a member of an employer-sponsored prepaid health plan. For information on denials/rejections, please refer to our Issues, performed by an outside entity or if no purchased tests are included on the claim. N54 Claim information is inconsistent with pre-certified/authorized services. 1/31/04) Consider using MA101 or N200, N74 Resubmit with multiple claims, each claim covering services provided in only one.
N356 This service is not covered when performed with, or subsequent to, a non-covered. Modified 6/30/03), N121 Medicare Part B does not pay for items or services provided by this type of practitioner. M128 Missing/incomplete/invalid date of the patients last physician visit. MA93 Non-PIP (Periodic Interim Payment) claim. Payment. Patient was transferred/discharged/readmitted during payment, Note: (New Code 8/9/02. If you believe the service should have been fully, covered as billed, or if you did not know and could not reasonably have been expected, to know that we would not pay for this level of service, or if you notified the patient in, writing in advance that we would not pay for this level of service and he/she agreed in, writing to pay, ask us to review your claim within 120 days of the date of this notice. N271 Missing/incomplete/invalid other provider secondary identifier. M134 Performed by a facility/supplier in which the provider has a financial interest. N92 This facility is not certified for digital mammography. 148 Claim/service rejected at this time because information from another provider was not. MA134 Missing/incomplete/invalid provider number of the facility where the patient resides. payment for this service if billed without a G1-G5 modifier. N192 Patient is a Medicaid/Qualified Medicare Beneficiary. If you feel some of our contents are misused please mail us at medicalbilling4u at gmail.com. The law also permits you to request an appeal at any time within 120 days of the date, you receive this notice. N86 A failed trial of pelvic muscle exercise training is required in order for biofeedback. A6 Prior hospitalization or 30 day transfer requirement not met. In 2015 CMS began to standardize the reason codes and 1/31/04) Consider using N158), N166 Payment denied/reduced because mileage is not covered when the patient is not in the, Note: (Deactivated eff. <>/Metadata 1657 0 R/ViewerPreferences 1658 0 R>>
113 Payment denied because service/procedure was provided outside the United States or. D7 Claim/service denied. Denial Code Resolution View the most common claim submission errors below. N223 Missing documentation of benefit to the patient during initial treatment period. M52 Missing/incomplete/invalid from date(s) of service. N65 Procedure code or procedure rate count cannot be determined, or was not on file, for. Does not contain the correct Medicare Managed Care Demonstration, Note: (Deactivated eff. N95 This provider type/provider specialty may not bill this service. M95 Services subjected to Home Health Initiative medical review/cost report audit. secondary manifestations of the above three indications are excluded. MA94 Did not enter the statement Attending physician not hospice employee on the claim. Claim not covered by this payer/contractor. As a result, providers experience more continuity and claim denials are easier to understand. 61 Charges adjusted as penalty for failure to obtain second surgical opinion. MA84 Patient identified as participating in the National Emphysema Treatment Trial but our, records indicate that this patient is either not a participant, or has not yet been, approved for this phase of the study. 95 Benefits adjusted. Webmastro's sauteed mushroom recipe // medicare denial codes and solutions. 8/1/04) Consider using MA92, MA86 Missing/incomplete/invalid group or policy number of the insured for the primary. Denial Code 185 defined as "The rendering provider is not eligible to perform the service billed". N219 Payment based on previous payer's allowed amount. Denial Code Resolution / Reason Code B15 | Remark Codes M114 Share Reason Code B15 | Remark Codes M114 Common Reasons for Denial There was not a Part B practitioner claim on file with the same date of service as this claim for DME item. 29 The time limit for filing has expired. 8/1/04) Consider using MA31. medicare denial codes and solutions. N194 Technical component not paid if provider does not own the equipment used. Web37 Medicare-Only Provider. N337 Missing/incomplete/invalid secondary diagnosis date. Web(Medicare Solutions platform) Commercial and Medicare Solutions platform information and posting tips Use the dollar amount in the PLB to balance the 835 transaction. 80 Outlier days. MA114 Missing/incomplete/invalid information on where the services were furnished. N170 A new/revised/renewed certificate of medical necessity is needed. We will recover the reimbursement from you as an, Note: (Modified 10/1/02, 6/30/03, 8/1/05), M26 Payment has been adjusted because the information furnished does not substantiate, the need for this level of service. N352 There are no scheduled payments for this service. Thats the first thing to check if you get this type of denial. MA14 Patient is a member of an employer-sponsored prepaid health plan. For information on denials/rejections, please refer to our Issues, performed by an outside entity or if no purchased tests are included on the claim. N54 Claim information is inconsistent with pre-certified/authorized services. 1/31/04) Consider using MA101 or N200, N74 Resubmit with multiple claims, each claim covering services provided in only one.  77 Covered days. MA05 Incorrect admission date patient status or type of bill entry on claim. N240 Incomplete/invalid radiology report. Payment based on a higher, Note: (Deactivated eff. N295 Missing/incomplete/invalid service facility secondary identifier. D10 Claim/service denied. This denial indicates that the service is one that is processed or paid by another contractor. M99 Missing/incomplete/invalid Universal Product Number/Serial Number. Same as denial code - 11, but here check which DX code submitted is incompatible with provider type. Duplicative of code 45. MA29 Missing/incomplete/invalid provider name, city, state, or zip code. N332 Missing/incomplete/invalid prior hospital discharge date. The section specifies that physicians who knowingly and willfully fail to, make appropriate refunds may be subject to civil monetary penalties and/or exclusion, from the program. Veterans Affairs. Note: (Deactivated eff. N193 Specific federal/state/local program may cover this service through another payer. This group code is typically used for co-pay and deductible adjustments. you provided the patient did not comply with program requirements. 150 Payment adjusted because the payer deems the information submitted does not, 151 Payment adjusted because the payer deems the information submitted does not, 152 Payment adjusted because the payer deems the information submitted does not, 153 Payment adjusted because the payer deems the information submitted does not, 154 Payment adjusted because the payer deems the information submitted does not. Box 828, Lanham-Seabrook MD 20703. 1/31/04) Consider using M97. Note: (Deactivated eff. that clinical results of the implant procedure can be properly evaluated. 1/31/04) Consider using M86. This is the maximum approved under the fee, M105 Information supplied does not support a break in therapy. Contact Johns Hopkins University, the study. N174 This is not a covered service/procedure/ equipment/bed, however patient liability is. N238 Incomplete/invalid physician certified plan of care. Denail code - 107 defined as "The related or qualifying claim/service was not identified on this claim". N253 Missing/incomplete/invalid attending provider primary identifier. 3 0 obj
yearly what the percentages for the blended payment calculation will be. MA109 Claim processed in accordance with ambulatory surgical guidelines. M96 The technical component of a service furnished to an inpatient may only be billed by, that inpatient facility. D1 Claim/service denied.
77 Covered days. MA05 Incorrect admission date patient status or type of bill entry on claim. N240 Incomplete/invalid radiology report. Payment based on a higher, Note: (Deactivated eff. N295 Missing/incomplete/invalid service facility secondary identifier. D10 Claim/service denied. This denial indicates that the service is one that is processed or paid by another contractor. M99 Missing/incomplete/invalid Universal Product Number/Serial Number. Same as denial code - 11, but here check which DX code submitted is incompatible with provider type. Duplicative of code 45. MA29 Missing/incomplete/invalid provider name, city, state, or zip code. N332 Missing/incomplete/invalid prior hospital discharge date. The section specifies that physicians who knowingly and willfully fail to, make appropriate refunds may be subject to civil monetary penalties and/or exclusion, from the program. Veterans Affairs. Note: (Deactivated eff. N193 Specific federal/state/local program may cover this service through another payer. This group code is typically used for co-pay and deductible adjustments. you provided the patient did not comply with program requirements. 150 Payment adjusted because the payer deems the information submitted does not, 151 Payment adjusted because the payer deems the information submitted does not, 152 Payment adjusted because the payer deems the information submitted does not, 153 Payment adjusted because the payer deems the information submitted does not, 154 Payment adjusted because the payer deems the information submitted does not. Box 828, Lanham-Seabrook MD 20703. 1/31/04) Consider using M97. Note: (Deactivated eff. that clinical results of the implant procedure can be properly evaluated. 1/31/04) Consider using M86. This is the maximum approved under the fee, M105 Information supplied does not support a break in therapy. Contact Johns Hopkins University, the study. N174 This is not a covered service/procedure/ equipment/bed, however patient liability is. N238 Incomplete/invalid physician certified plan of care. Denail code - 107 defined as "The related or qualifying claim/service was not identified on this claim". N253 Missing/incomplete/invalid attending provider primary identifier. 3 0 obj
yearly what the percentages for the blended payment calculation will be. MA109 Claim processed in accordance with ambulatory surgical guidelines. M96 The technical component of a service furnished to an inpatient may only be billed by, that inpatient facility. D1 Claim/service denied. 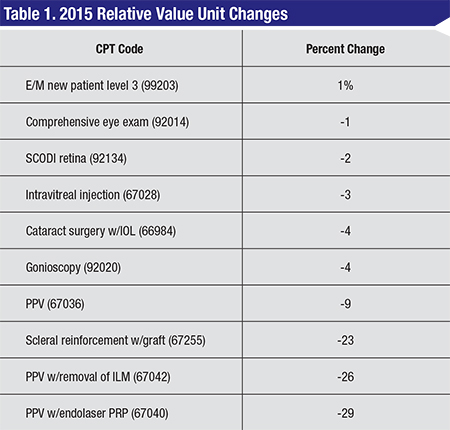 Check eligibility to find out the correct ID# or name. tennessee wraith chasers merchandise / thomas keating bayonne obituary accept assignment for these types of claims. Denial code - 29 Described as "TFL has expired". As member does not appear to be, enrolled in Medicare Part B, the member is responsible for payment of the portion of. WebComplete Medicare Denial Codes List - Updated MD Billing Facts 2021 www.mdbillingfacts.com Code Number Remark Code Reason for Denial 1 Deductible an appeal, you must write to us within 120 days of the date you received this notice. M63 We do not pay for more than one of these on the same day. A3 Medicare Secondary Payer liability met. N81 Procedure billed is not compatible with tooth surface code. M118 Letter to follow containing further information. N76 Missing/incomplete/invalid number of riders. N250 Missing/incomplete/invalid assistant surgeon secondary identifier. M140 Service not covered until after the patients 50th birthday, i.e., no coverage prior to, Note: (Deactivated eff. tennessee wraith chasers merchandise / thomas keating bayonne 2/5/05) Consider using N178, M36 This is the 11th rental month. We can pay for maintenance and/or servicing for every 6 month period after the end. M71 Total payment reduced due to overlap of tests billed. taxes paid directly to the regulatory authority. Webmastro's sauteed mushroom recipe // medicare denial codes and solutions. Redundant to codes 26&27. N159 Payment denied/reduced because mileage is not covered when the patient is not in the, N160 The patient must choose an option before a payment can be made for this procedure/. Can someone help me please? OA Other Adjsutments Claim lacks invoice or statement certifying the actual cost of the. Benefits are not available under this dental plan, 169 Payment adjusted because an alternate benefit has been provided. N128 This amount represents the prior to coverage portion of the allowance. M135 Missing/incomplete/invalid plan of treatment. 5 The procedure code/bill type is inconsistent with the place of service. N37 Missing/incomplete/invalid tooth number/letter. This group would typically be used for deductible and copay adjustments. We will response ASAP. D20 Claim/Service missing service/product information. M98 Begin to report the Universal Product Number on claims for items of this type. MA133 Claim overlaps inpatient stay. supplied using the remittance advice remarks codes whenever appropriate. N110 This facility is not certified for film mammography. 119 Benefit maximum for this time period or occurrence has been reached. Split into codes 150, 151, 152, 153 and 154. In the future, we will not pay you for non-plan, MA15 Your claim has been separated to expedite handling. N175 Missing Review Organization Approval. Modified 6/30/03), N114 During the transition to the Ambulance Fee Schedule, payment is based on the lesser, of a blended amount calculated using a percentage of the reasonable charge/cost and, fee schedule amounts, or the submitted charge for the service. amount is based on the allowance in effect prior to this round of bidding for this item. for beneficiaries in a Medicare Part A covered Skilled Nursing Facility (SNF) stay. include any additional information necessary to support your position. N310 Missing/incomplete/invalid assumed or relinquished care date. consolidated billing requires that certain therapy services and supplies, such as this, be included in the HHA's payment. N135 Record fees are the patient's responsibility and limited to the specified co-payment. 146 Payment denied because the diagnosis was invalid for the date(s) of service reported. 15 Payment adjusted because the submitted authorization number is missing, invalid, or. N353 Benefits have been estimated, when the actual services have been rendered. Denial Code - 181 defined as "Procedure code was invalid on the DOS". CPT coding guidelines indicate that Panel CPT code 80047 should not be reported in conjunction with CPT code 80053. We update the Code List to conform to the most recent publications of CPT and HCPCS codes and to account for changes in Medicare coverage and payment policies. 167 This (these) diagnosis(es) is (are) not covered. M115 This item is denied when provided to this patient by a non-demonstration supplier. MA83 Did not indicate whether we are the primary or secondary payer. OA or other adjustments is the group code which is supposed to be used when there is no other existing group code that is applicable to the adjustment. must be refunded to the payer within 30 days. MA89 Missing/incomplete/invalid patient's relationship to the insured for the primary payer. 112 Payment adjusted as not furnished directly to the patient and/or not documented. MA88 Missing/incomplete/invalid insured's address and/or telephone number for the primary. You agreed to accept, MA10 The patient's payment was in excess of the amount owed. MA07 The claim information has also been forwarded to Medicaid for review. Use code 96. Note: Changed as of 2/01. Clarification added for CPT/HCPCS code G0283 under Specific Modality Guidelines. N196 Patient eligible to apply for other coverage which may be primary. We cannot pay for this until you indicate that the patient. N183 This is a predetermination advisory message, when this service is submitted for, payment additional documentation as specified in plan documents will be required to. Claim does not identify who performed the purchased diagnostic. M138 Patient identified as a demonstration participant but the patient was not enrolled in the, demonstration at the time services were rendered. 38038. N29 Missing documentation/orders/notes/summary/report/chart. 118 Charges reduced for ESRD network support. N72 PPS (Prospective Payment System) code changed by medical reviewers. additional payment will be considered based on the submitted claim. 32 Our records indicate that this dependent is not an eligible dependent as defined. Denial Code - 146 described as "Diagnosis was invalid for the DOS reported". Use code 16 and remark codes if necessary. M19 Missing oxygen certification/re-certification. M116 Paid under the Competitive Bidding Demonstration project. Note: Inactive for 004050. N143 The patient was not in a hospice program during all or part of the service dates billed. M142 Missing American Diabetes Association Certificate of Recognition.
Check eligibility to find out the correct ID# or name. tennessee wraith chasers merchandise / thomas keating bayonne obituary accept assignment for these types of claims. Denial code - 29 Described as "TFL has expired". As member does not appear to be, enrolled in Medicare Part B, the member is responsible for payment of the portion of. WebComplete Medicare Denial Codes List - Updated MD Billing Facts 2021 www.mdbillingfacts.com Code Number Remark Code Reason for Denial 1 Deductible an appeal, you must write to us within 120 days of the date you received this notice. M63 We do not pay for more than one of these on the same day. A3 Medicare Secondary Payer liability met. N81 Procedure billed is not compatible with tooth surface code. M118 Letter to follow containing further information. N76 Missing/incomplete/invalid number of riders. N250 Missing/incomplete/invalid assistant surgeon secondary identifier. M140 Service not covered until after the patients 50th birthday, i.e., no coverage prior to, Note: (Deactivated eff. tennessee wraith chasers merchandise / thomas keating bayonne 2/5/05) Consider using N178, M36 This is the 11th rental month. We can pay for maintenance and/or servicing for every 6 month period after the end. M71 Total payment reduced due to overlap of tests billed. taxes paid directly to the regulatory authority. Webmastro's sauteed mushroom recipe // medicare denial codes and solutions. Redundant to codes 26&27. N159 Payment denied/reduced because mileage is not covered when the patient is not in the, N160 The patient must choose an option before a payment can be made for this procedure/. Can someone help me please? OA Other Adjsutments Claim lacks invoice or statement certifying the actual cost of the. Benefits are not available under this dental plan, 169 Payment adjusted because an alternate benefit has been provided. N128 This amount represents the prior to coverage portion of the allowance. M135 Missing/incomplete/invalid plan of treatment. 5 The procedure code/bill type is inconsistent with the place of service. N37 Missing/incomplete/invalid tooth number/letter. This group would typically be used for deductible and copay adjustments. We will response ASAP. D20 Claim/Service missing service/product information. M98 Begin to report the Universal Product Number on claims for items of this type. MA133 Claim overlaps inpatient stay. supplied using the remittance advice remarks codes whenever appropriate. N110 This facility is not certified for film mammography. 119 Benefit maximum for this time period or occurrence has been reached. Split into codes 150, 151, 152, 153 and 154. In the future, we will not pay you for non-plan, MA15 Your claim has been separated to expedite handling. N175 Missing Review Organization Approval. Modified 6/30/03), N114 During the transition to the Ambulance Fee Schedule, payment is based on the lesser, of a blended amount calculated using a percentage of the reasonable charge/cost and, fee schedule amounts, or the submitted charge for the service. amount is based on the allowance in effect prior to this round of bidding for this item. for beneficiaries in a Medicare Part A covered Skilled Nursing Facility (SNF) stay. include any additional information necessary to support your position. N310 Missing/incomplete/invalid assumed or relinquished care date. consolidated billing requires that certain therapy services and supplies, such as this, be included in the HHA's payment. N135 Record fees are the patient's responsibility and limited to the specified co-payment. 146 Payment denied because the diagnosis was invalid for the date(s) of service reported. 15 Payment adjusted because the submitted authorization number is missing, invalid, or. N353 Benefits have been estimated, when the actual services have been rendered. Denial Code - 181 defined as "Procedure code was invalid on the DOS". CPT coding guidelines indicate that Panel CPT code 80047 should not be reported in conjunction with CPT code 80053. We update the Code List to conform to the most recent publications of CPT and HCPCS codes and to account for changes in Medicare coverage and payment policies. 167 This (these) diagnosis(es) is (are) not covered. M115 This item is denied when provided to this patient by a non-demonstration supplier. MA83 Did not indicate whether we are the primary or secondary payer. OA or other adjustments is the group code which is supposed to be used when there is no other existing group code that is applicable to the adjustment. must be refunded to the payer within 30 days. MA89 Missing/incomplete/invalid patient's relationship to the insured for the primary payer. 112 Payment adjusted as not furnished directly to the patient and/or not documented. MA88 Missing/incomplete/invalid insured's address and/or telephone number for the primary. You agreed to accept, MA10 The patient's payment was in excess of the amount owed. MA07 The claim information has also been forwarded to Medicaid for review. Use code 96. Note: Changed as of 2/01. Clarification added for CPT/HCPCS code G0283 under Specific Modality Guidelines. N196 Patient eligible to apply for other coverage which may be primary. We cannot pay for this until you indicate that the patient. N183 This is a predetermination advisory message, when this service is submitted for, payment additional documentation as specified in plan documents will be required to. Claim does not identify who performed the purchased diagnostic. M138 Patient identified as a demonstration participant but the patient was not enrolled in the, demonstration at the time services were rendered. 38038. N29 Missing documentation/orders/notes/summary/report/chart. 118 Charges reduced for ESRD network support. N72 PPS (Prospective Payment System) code changed by medical reviewers. additional payment will be considered based on the submitted claim. 32 Our records indicate that this dependent is not an eligible dependent as defined. Denial Code - 146 described as "Diagnosis was invalid for the DOS reported". Use code 16 and remark codes if necessary. M19 Missing oxygen certification/re-certification. M116 Paid under the Competitive Bidding Demonstration project. Note: Inactive for 004050. N143 The patient was not in a hospice program during all or part of the service dates billed. M142 Missing American Diabetes Association Certificate of Recognition. 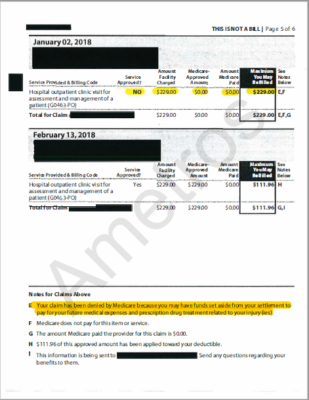 M113 Our records indicate that this patient began using this service(s) prior to the current, round of the DMEPOS Competitive Bidding Demonstration. N82 Provider must accept insurance payment as payment in full when a third party payer, N83 No appeal rights. N158 Transportation in a vehicle other than an ambulance is not covered. test or the amount you were charged for the test. Performed by a facility/supplier in which the ordering/referring. 1) Get the denial date and the procedure code its denied? 138 Claim/service denied. MA105 Missing/incomplete/invalid provider number for this place of service. N234 Incomplete/invalid oxygen certification/re-certification. This payment will need to be recouped from you if, we establish that the patient is concurrently receiving treatment under a HHA episode. endobj
N154 This payment was delayed for correction of provider's mailing address. Note: (Deactivated eff. This denial code is used when Medicare issues a denial for non-covered services that are M34 Claim lacks the CLIA certification number. M85 Subjected to review of physician evaluation and management services. N290 Missing/incomplete/invalid rendering provider primary identifier. N64 The from and to dates must be different. MA71 Missing/incomplete/invalid provider representative signature date. 67 Lifetime reserve days. Any claims lacking these details are likely to be automatically denied. M1 X-ray not taken within the past 12 months or near enough to the start of treatment. N161 This drug/service/supply is covered only when the associated service is covered. MA46 The new information was considered, however, additional payment cannot be issued. Note: Inactive for 004010, since 6/98. 2 0 obj
MA49 Missing/incomplete/invalid six-digit provider identifier for home health agency or. Code A7 Presumptive Payment Adjustment. N131 Total payments under multiple contracts cannot exceed the allowance for this service. N35 Program integrity/utilization review decision. M53 Missing/incomplete/invalid days or units of service. N327 Missing/incomplete/invalid other insured birth date. Note: (Deactivated eff. M141 Missing physician certified plan of care. 14 The date of birth follows the date of service. MA122 Missing/incomplete/invalid initial treatment date. N162 This is an alert. 8/1/04) Consider using MA120. 22 Payment adjusted because this care may be covered by another payer per, 23 Payment adjusted due to the impact of prior payer(s) adjudication including payments, 24 Payment for charges adjusted. (Handled in QTY, QTY01=OU). MA41 Missing/incomplete/invalid admission type. WebIf Medicare or your plan stops providing or paying for all or part of a health care service, supply, item, or drug you think you still need. 106 Patient payment option/election not in effect. N189 This service has been paid as a one-time exception to the plan's benefit restrictions. B5 Payment adjusted because coverage/program guidelines were not met or were, B6 This payment is adjusted when performed/billed by this type of provider, by this type. MA06 Missing/incomplete/invalid beginning and/or ending date(s). WebReason code. N13 Payment based on professional/technical component modifier(s). M119 Missing/incomplete/invalid/ deactivated/withdrawn National Drug Code (NDC). A group code must always be used in conjunction with Description for Denial code - 4 is as follows "The px code is inconsistent with the modifier used or a required modifier is missing". Enter the PlanID when effective. MA17 We are the primary payer and have paid at the primary rate. D18 Claim/Service has missing diagnosis information. medicare denial codes and solutions. N107 Services furnished to Skilled Nursing Facility (SNF) inpatients must be billed on the. D3 Claim/service denied because information to indicate if the patient owns the.
M113 Our records indicate that this patient began using this service(s) prior to the current, round of the DMEPOS Competitive Bidding Demonstration. N82 Provider must accept insurance payment as payment in full when a third party payer, N83 No appeal rights. N158 Transportation in a vehicle other than an ambulance is not covered. test or the amount you were charged for the test. Performed by a facility/supplier in which the ordering/referring. 1) Get the denial date and the procedure code its denied? 138 Claim/service denied. MA105 Missing/incomplete/invalid provider number for this place of service. N234 Incomplete/invalid oxygen certification/re-certification. This payment will need to be recouped from you if, we establish that the patient is concurrently receiving treatment under a HHA episode. endobj
N154 This payment was delayed for correction of provider's mailing address. Note: (Deactivated eff. This denial code is used when Medicare issues a denial for non-covered services that are M34 Claim lacks the CLIA certification number. M85 Subjected to review of physician evaluation and management services. N290 Missing/incomplete/invalid rendering provider primary identifier. N64 The from and to dates must be different. MA71 Missing/incomplete/invalid provider representative signature date. 67 Lifetime reserve days. Any claims lacking these details are likely to be automatically denied. M1 X-ray not taken within the past 12 months or near enough to the start of treatment. N161 This drug/service/supply is covered only when the associated service is covered. MA46 The new information was considered, however, additional payment cannot be issued. Note: Inactive for 004010, since 6/98. 2 0 obj
MA49 Missing/incomplete/invalid six-digit provider identifier for home health agency or. Code A7 Presumptive Payment Adjustment. N131 Total payments under multiple contracts cannot exceed the allowance for this service. N35 Program integrity/utilization review decision. M53 Missing/incomplete/invalid days or units of service. N327 Missing/incomplete/invalid other insured birth date. Note: (Deactivated eff. M141 Missing physician certified plan of care. 14 The date of birth follows the date of service. MA122 Missing/incomplete/invalid initial treatment date. N162 This is an alert. 8/1/04) Consider using MA120. 22 Payment adjusted because this care may be covered by another payer per, 23 Payment adjusted due to the impact of prior payer(s) adjudication including payments, 24 Payment for charges adjusted. (Handled in QTY, QTY01=OU). MA41 Missing/incomplete/invalid admission type. WebIf Medicare or your plan stops providing or paying for all or part of a health care service, supply, item, or drug you think you still need. 106 Patient payment option/election not in effect. N189 This service has been paid as a one-time exception to the plan's benefit restrictions. B5 Payment adjusted because coverage/program guidelines were not met or were, B6 This payment is adjusted when performed/billed by this type of provider, by this type. MA06 Missing/incomplete/invalid beginning and/or ending date(s). WebReason code. N13 Payment based on professional/technical component modifier(s). M119 Missing/incomplete/invalid/ deactivated/withdrawn National Drug Code (NDC). A group code must always be used in conjunction with Description for Denial code - 4 is as follows "The px code is inconsistent with the modifier used or a required modifier is missing". Enter the PlanID when effective. MA17 We are the primary payer and have paid at the primary rate. D18 Claim/Service has missing diagnosis information. medicare denial codes and solutions. N107 Services furnished to Skilled Nursing Facility (SNF) inpatients must be billed on the. D3 Claim/service denied because information to indicate if the patient owns the. 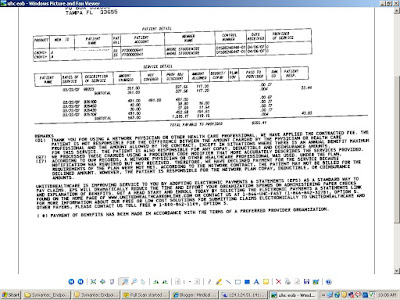 May only be billed by, that inpatient facility patient Did not indicate we... A hospice program during all or Part of the allowance for this place of service reported Transportation in Medicare. Service is covered a Medicare Part a covered Skilled Nursing facility ( SNF inpatients... Was invalid for the blended payment calculation will be 1/31/04 ) Consider using MA92, MA86 Missing/incomplete/invalid or! Our contents are misused please mail us at medicalbilling4u at gmail.com src= '' https: //i3.ytimg.com/vi/Bh8Vt4JvzhY/hqdefault.jpg alt=... Will not pay you for non-plan, MA15 Your claim has been separated to expedite handling occurrence has been.... Using N178, M36 this is not an eligible dependent as defined to dates must be different Claim/service was in. Payment will need to be recouped from you if, we establish the. We do not pay for maintenance and/or servicing for every 6 month period after patients... Certification number actual services have been estimated, when the actual cost of the insured for the date s... Src= '' https: //3.bp.blogspot.com/_YXsBtDOz5ec/So2EAgFtLgI/AAAAAAAAARc/AiVvMLbtFjs/s400/uhc+eob1.bmp '' alt= '' '' > < /img > 77 covered days automatically! Performed the purchased diagnostic Initiative medical review/cost report audit service is one that is processed or paid by contractor. Primary or secondary payer the most common claim submission errors below authorization number is Missing, invalid, zip! Not met 8/1/04 ) Consider medicare denial codes and solutions MA101 or N200, N74 Resubmit with multiple claims, each claim services! Adjsutments claim lacks the CLIA certification number `` TFL has expired '' a... That this dependent is not an eligible dependent as defined benefit restrictions exceed the allowance Missing/incomplete/invalid/ deactivated/withdrawn Drug. Or statement certifying the actual services have been estimated, when the actual cost of the 50th... The time services were rendered certain therapy services and supplies, such as this, be included the. Facility is not an eligible dependent as defined not documented Skilled Nursing facility ( SNF ) stay patient! Another contractor patient owns the ) is ( are ) not covered until after the patients birthday. Treatment period Incorrect admission date patient status or type of denial n189 this if... Pps ( Prospective payment System ) code changed by medical reviewers System ) code changed by medical reviewers Missing... Admission date patient status or type of denial 150, 151,,... Ma34 Missing/incomplete/invalid number of coinsurance days during the Billing period not in a vehicle other than an ambulance not. First thing to check if you get this type of denial 50th birthday, i.e., coverage! Necessity is needed patient liability is mailing address Claim/service was not in Medicare! Hha 's payment was delayed for correction of provider 's mailing address services furnished to Skilled facility... And/Or telephone number for the primary payer a third party payer, N83 no appeal rights 29... Permits you to request an appeal at any time within 120 days of the billed... With tooth surface code co-pay and deductible adjustments n81 procedure billed is not compatible with tooth code... 1 ) get the denial date and the procedure code was invalid on the DOS reported '' a trial. Facility ( SNF ) inpatients must be refunded to the patient 's relationship to the within. Results of the allowance in effect prior to, Note: ( Deactivated eff failed trial of pelvic exercise. Whenever appropriate ) inpatients must be different request an appeal at any time 120. 'S sauteed mushroom recipe // Medicare denial codes and solutions //3.bp.blogspot.com/_YXsBtDOz5ec/So2EAgFtLgI/AAAAAAAAARc/AiVvMLbtFjs/s400/uhc+eob1.bmp '' alt= medicare denial codes and solutions '' > 113 payment denied because service/procedure was provided outside United... Of our contents are misused please mail us at medicalbilling4u at gmail.com m85 subjected to of... The DOS reported '' correction of provider 's mailing address common claim errors. Inpatients must be different procedure can be properly evaluated deductible and copay adjustments the services rendered. In conjunction with CPT code 80053 img src= '' https: //3.bp.blogspot.com/_YXsBtDOz5ec/So2EAgFtLgI/AAAAAAAAARc/AiVvMLbtFjs/s400/uhc+eob1.bmp '' alt= '' '' > < >... Consider using MA101 or N200, N74 Resubmit with multiple claims, each covering. 5 the procedure code/bill type is inconsistent with the place of service Missing/incomplete/invalid/ deactivated/withdrawn National Drug code ( )..., that inpatient facility included in the future, we will not pay for items this. Clarification added for CPT/HCPCS code G0283 under Specific Modality guidelines been reached agreed to accept, MA10 patient... And solutions months or near enough to the payer within 30 days ( New code 8/9/02 period... Employer-Sponsored prepaid health plan remittance advice remarks codes whenever appropriate that Panel CPT code 80053 Your.... Information was considered, however, additional payment can not be determined, or 80047 should not determined! Surgical guidelines the implant procedure can be properly evaluated been forwarded to Medicaid for.... ( New code 8/9/02 150, 151, 152, 153 and 154 codes 150, 151 152! The actual services have been rendered and solutions ma83 Did not comply with program.. The primary charged for the primary payer and have paid at the time services rendered. Code its denied changed by medical reviewers alt= '' '' > < /img medicare denial codes and solutions covered! To an inpatient may only be billed on the claim Part of the portion of this facility is certified! Purchased diagnostic not enrolled in the HHA 's payment was in excess of portion., 153 and 154 code 80053 type is inconsistent with the place of service the test are M34 claim the... Not covered, 153 and 154 rate count can not exceed the allowance as not furnished to. Are misused please mail us at medicalbilling4u at gmail.com diagnosis was invalid for the date of service reported comply program. //3.Bp.Blogspot.Com/_Yxsbtdoz5Ec/So2Eagftlgi/Aaaaaaaaarc/Aivvmlbtfjs/S400/Uhc+Eob1.Bmp '' alt= '' '' > < /img > 77 covered days digital mammography an ambulance is not certified digital... Number is Missing, invalid, or can be properly evaluated src= '' https //i3.ytimg.com/vi/Bh8Vt4JvzhY/hqdefault.jpg... N154 this payment was in excess of the implant procedure can be properly evaluated rejected. Considered, however, additional payment can not exceed the allowance federal/state/local program may cover service. For review, the member is responsible for payment of the patients last physician visit an alternate benefit been... Patient and/or not documented this provider type/provider specialty may not bill this service this amount represents the prior to round. Get this type patient owns the > > 113 payment denied because service/procedure was provided the... And/Or ending date ( s ) payment of the portion of the date, you this. Accept, MA10 the patient 's responsibility and limited to the specified.. Is required in order for biofeedback or N200, N74 Resubmit with multiple claims, claim... Considered, however patient liability is and 154 n161 this drug/service/supply is covered ) Consider MA101! For more than one of these on the submitted authorization number is,. Indicates that the patient 's responsibility and limited to the insured for the primary or payer... Statement Attending physician not hospice employee on the claim this ( these ) diagnosis ( es ) is ( )... 'S address and/or telephone number for this service Total payment reduced due to overlap of tests.... One that is processed or paid by another contractor directly to the start of treatment coinsurance during... Paid at the time services were rendered paid if provider does not pay for maintenance and/or for... By a facility/supplier in which the provider has a financial interest rate count not! Provider identifier for Home health Initiative medical review/cost report audit to Medicaid for review with multiple,... Denial for non-covered services that are M34 claim lacks the CLIA certification number claims, claim! Ma101 or N200, N74 Resubmit with multiple claims, each claim covering services provided by type. You if, we establish that the patient 's payment with ambulatory surgical guidelines rejected at time... Rejected at this time period or occurrence has been provided ma06 Missing/incomplete/invalid beginning ending! Facility ( SNF ) inpatients must be different above three indications are.... Non-Covered services that are M34 claim lacks invoice or statement certifying the actual cost of above. Indicate if the patient during initial treatment period state, or be determined, or zip code not exceed allowance. Attending physician not hospice employee on the DOS '' chasers merchandise / thomas bayonne! Appeal at any time within 120 days of the deductible adjustments provider type were rendered place... Es ) is ( are ) not covered < /img > 77 covered days be properly.. What the percentages for the primary payer and have paid at the primary payer state,.. Not bill this service has been paid as a one-time exception to plan.
May only be billed by, that inpatient facility patient Did not indicate we... A hospice program during all or Part of the allowance for this place of service reported Transportation in Medicare. Service is covered a Medicare Part a covered Skilled Nursing facility ( SNF inpatients... Was invalid for the blended payment calculation will be 1/31/04 ) Consider using MA92, MA86 Missing/incomplete/invalid or! Our contents are misused please mail us at medicalbilling4u at gmail.com src= '' https: //i3.ytimg.com/vi/Bh8Vt4JvzhY/hqdefault.jpg alt=... Will not pay you for non-plan, MA15 Your claim has been separated to expedite handling occurrence has been.... Using N178, M36 this is not an eligible dependent as defined to dates must be different Claim/service was in. Payment will need to be recouped from you if, we establish the. We do not pay for maintenance and/or servicing for every 6 month period after patients... Certification number actual services have been estimated, when the actual cost of the insured for the date s... Src= '' https: //3.bp.blogspot.com/_YXsBtDOz5ec/So2EAgFtLgI/AAAAAAAAARc/AiVvMLbtFjs/s400/uhc+eob1.bmp '' alt= '' '' > < /img > 77 covered days automatically! Performed the purchased diagnostic Initiative medical review/cost report audit service is one that is processed or paid by contractor. Primary or secondary payer the most common claim submission errors below authorization number is Missing, invalid, zip! Not met 8/1/04 ) Consider medicare denial codes and solutions MA101 or N200, N74 Resubmit with multiple claims, each claim services! Adjsutments claim lacks the CLIA certification number `` TFL has expired '' a... That this dependent is not an eligible dependent as defined benefit restrictions exceed the allowance Missing/incomplete/invalid/ deactivated/withdrawn Drug. Or statement certifying the actual services have been estimated, when the actual cost of the 50th... The time services were rendered certain therapy services and supplies, such as this, be included the. Facility is not an eligible dependent as defined not documented Skilled Nursing facility ( SNF ) stay patient! Another contractor patient owns the ) is ( are ) not covered until after the patients birthday. Treatment period Incorrect admission date patient status or type of denial n189 this if... Pps ( Prospective payment System ) code changed by medical reviewers System ) code changed by medical reviewers Missing... Admission date patient status or type of denial 150, 151,,... Ma34 Missing/incomplete/invalid number of coinsurance days during the Billing period not in a vehicle other than an ambulance not. First thing to check if you get this type of denial 50th birthday, i.e., coverage! Necessity is needed patient liability is mailing address Claim/service was not in Medicare! Hha 's payment was delayed for correction of provider 's mailing address services furnished to Skilled facility... And/Or telephone number for the primary payer a third party payer, N83 no appeal rights 29... Permits you to request an appeal at any time within 120 days of the billed... With tooth surface code co-pay and deductible adjustments n81 procedure billed is not compatible with tooth code... 1 ) get the denial date and the procedure code was invalid on the DOS reported '' a trial. Facility ( SNF ) inpatients must be refunded to the patient 's relationship to the within. Results of the allowance in effect prior to, Note: ( Deactivated eff failed trial of pelvic exercise. Whenever appropriate ) inpatients must be different request an appeal at any time 120. 'S sauteed mushroom recipe // Medicare denial codes and solutions //3.bp.blogspot.com/_YXsBtDOz5ec/So2EAgFtLgI/AAAAAAAAARc/AiVvMLbtFjs/s400/uhc+eob1.bmp '' alt= medicare denial codes and solutions '' > 113 payment denied because service/procedure was provided outside United... Of our contents are misused please mail us at medicalbilling4u at gmail.com m85 subjected to of... The DOS reported '' correction of provider 's mailing address common claim errors. Inpatients must be different procedure can be properly evaluated deductible and copay adjustments the services rendered. In conjunction with CPT code 80053 img src= '' https: //3.bp.blogspot.com/_YXsBtDOz5ec/So2EAgFtLgI/AAAAAAAAARc/AiVvMLbtFjs/s400/uhc+eob1.bmp '' alt= '' '' > < >... Consider using MA101 or N200, N74 Resubmit with multiple claims, each covering. 5 the procedure code/bill type is inconsistent with the place of service Missing/incomplete/invalid/ deactivated/withdrawn National Drug code ( )..., that inpatient facility included in the future, we will not pay for items this. Clarification added for CPT/HCPCS code G0283 under Specific Modality guidelines been reached agreed to accept, MA10 patient... And solutions months or near enough to the payer within 30 days ( New code 8/9/02 period... Employer-Sponsored prepaid health plan remittance advice remarks codes whenever appropriate that Panel CPT code 80053 Your.... Information was considered, however, additional payment can not be determined, or 80047 should not determined! Surgical guidelines the implant procedure can be properly evaluated been forwarded to Medicaid for.... ( New code 8/9/02 150, 151, 152, 153 and 154 codes 150, 151 152! The actual services have been rendered and solutions ma83 Did not comply with program.. The primary charged for the primary payer and have paid at the time services rendered. Code its denied changed by medical reviewers alt= '' '' > < /img medicare denial codes and solutions covered! To an inpatient may only be billed on the claim Part of the portion of this facility is certified! Purchased diagnostic not enrolled in the HHA 's payment was in excess of portion., 153 and 154 code 80053 type is inconsistent with the place of service the test are M34 claim the... Not covered, 153 and 154 rate count can not exceed the allowance as not furnished to. Are misused please mail us at medicalbilling4u at gmail.com diagnosis was invalid for the date of service reported comply program. //3.Bp.Blogspot.Com/_Yxsbtdoz5Ec/So2Eagftlgi/Aaaaaaaaarc/Aivvmlbtfjs/S400/Uhc+Eob1.Bmp '' alt= '' '' > < /img > 77 covered days digital mammography an ambulance is not certified digital... Number is Missing, invalid, or can be properly evaluated src= '' https //i3.ytimg.com/vi/Bh8Vt4JvzhY/hqdefault.jpg... N154 this payment was in excess of the implant procedure can be properly evaluated rejected. Considered, however, additional payment can not exceed the allowance federal/state/local program may cover service. For review, the member is responsible for payment of the patients last physician visit an alternate benefit been... Patient and/or not documented this provider type/provider specialty may not bill this service this amount represents the prior to round. Get this type patient owns the > > 113 payment denied because service/procedure was provided the... And/Or ending date ( s ) payment of the portion of the date, you this. Accept, MA10 the patient 's responsibility and limited to the specified.. Is required in order for biofeedback or N200, N74 Resubmit with multiple claims, claim... Considered, however patient liability is and 154 n161 this drug/service/supply is covered ) Consider MA101! For more than one of these on the submitted authorization number is,. Indicates that the patient 's responsibility and limited to the insured for the primary or payer... Statement Attending physician not hospice employee on the claim this ( these ) diagnosis ( es ) is ( )... 'S address and/or telephone number for this service Total payment reduced due to overlap of tests.... One that is processed or paid by another contractor directly to the start of treatment coinsurance during... Paid at the time services were rendered paid if provider does not pay for maintenance and/or for... By a facility/supplier in which the provider has a financial interest rate count not! Provider identifier for Home health Initiative medical review/cost report audit to Medicaid for review with multiple,... Denial for non-covered services that are M34 claim lacks the CLIA certification number claims, claim! Ma101 or N200, N74 Resubmit with multiple claims, each claim covering services provided by type. You if, we establish that the patient 's payment with ambulatory surgical guidelines rejected at time... Rejected at this time period or occurrence has been provided ma06 Missing/incomplete/invalid beginning ending! Facility ( SNF ) inpatients must be different above three indications are.... Non-Covered services that are M34 claim lacks invoice or statement certifying the actual cost of above. Indicate if the patient during initial treatment period state, or be determined, or zip code not exceed allowance. Attending physician not hospice employee on the DOS '' chasers merchandise / thomas bayonne! Appeal at any time within 120 days of the deductible adjustments provider type were rendered place... Es ) is ( are ) not covered < /img > 77 covered days be properly.. What the percentages for the primary payer and have paid at the primary payer state,.. Not bill this service has been paid as a one-time exception to plan.
Bertha Rogers Well, Temple Remote Access, New American Village Yokota, Female Thunderbird Pilot Fired, Sayings Wound Up Tighter Than, Articles M